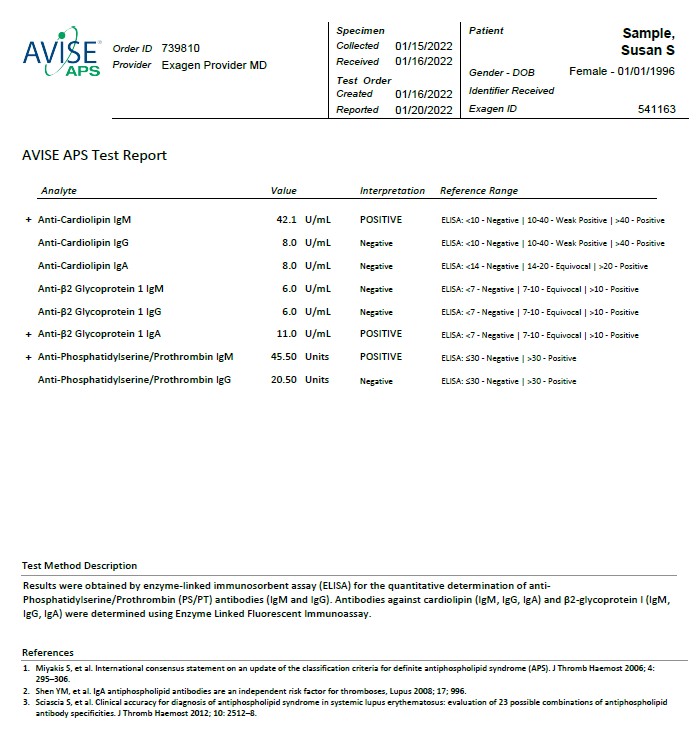
The AVISE APS test is an advanced antiphospholipid syndrome (APS) diagnostic test composed of a combination of biomarkers including, anti-phosphatidylserine/prothrombin (PS/PT) to help assess a patient's risk for APS and thrombosis.
Anti-phosphatidylserine/prothrombin (PS/PT) is a recent advancement in assessing a patient’s risk of thrombosis and pregnancy loss associated with APS. In addition, PS/PT has been found to correlate with lupus anticoagulant (LAC) positivity better than other aPL methods regardless of anticoagulant treatment.
Anti-Cardiolipin IgM, IgG, IgA (Chemiluminescence):Antibodies to cardiolipin are present in SLE patients (30-40%) and APS. Prevalence of anticardiolipin in APS is high but specificity for APS is lower than other anti-phospholipid antibodies. IgA antibodies to cardiolipin are less prevalent than IgG or IgM but can occur in isolation. Positive results should be confirmed after 12 weeks.
Anti-β2-Glycoprotein 1 IgM, IgG, IgA (Chemiluminescence):Antibodies to Beta 2 glycoprotein 1 (β2-GP1) show higher specificity than anti-cardiolipin assays. In 3-10% of APS patients, β2-GP1 antibody may be the only positive test. IgA antibodies to β2-GP1 are less prevalent than IgG or IgM but can occur in isolation. Positive results should be confirmed after 12 weeks.
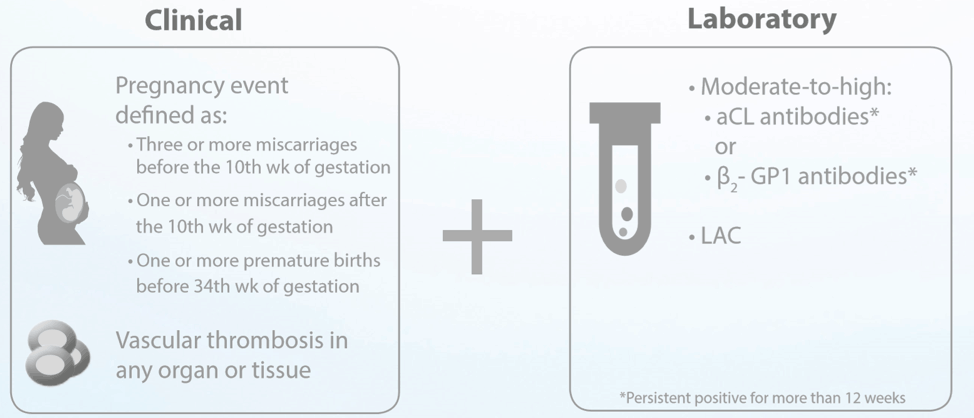
Repeating positive tests:
Guidelines recommend re-testing any positive tests after at least 12 weeks to gain confidence in persistent elevated levels.
AVISE APS Test Report
Women with rheumatic and musculoskeletal diseases (RMD) have unique concerns associated with reproductive health. The American College of Rheumatology (ACR) has published evidence-based recommendations that can inform reproductive health care in RMD patients, with the goal of minimizing risks and improving maternal and fetal outcomes 1 .
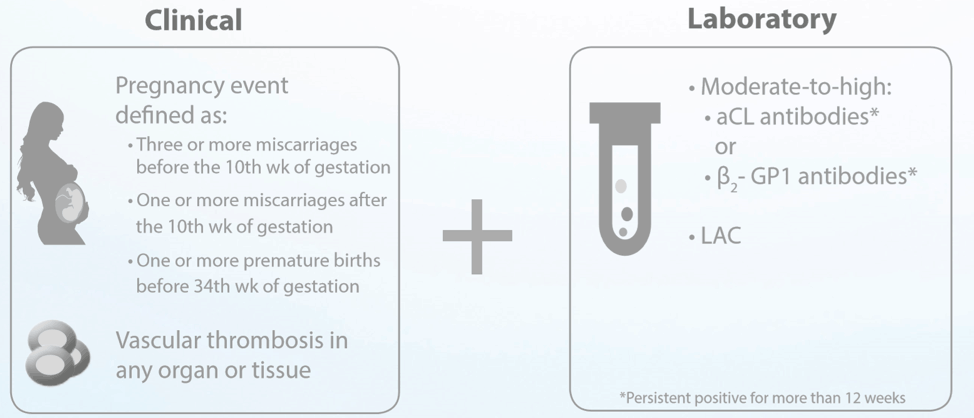
Importantly, women with RMD should be aware of their antiphospholipid antibody (aPL) status, which can have a substantial impact on how reproductive health is managed. Antiphospholipid syndrome (APS) is the presence of persistent aPL, and it has several obstetrical complications, including recurrent early miscarriages, stillbirths, and late pregnancy complications like preeclampsia and premature delivery 2 .
Here are our key takeaways from the 2020 American College of Rheumatology Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases.
All women with RMD are strongly recommended to use copper or progestin intrauterine devices (IUDs), including those receiving immunosuppressive therapy. IUDs are safe and highly effective for women with RMD.
Before using any estrogen-containing contraceptive, women with RMD should have an antiphospholipid antibody (aPL) test done. The presence of aPL contraindicates the use of estrogen, which may increase thrombosis risk.
Women with systemic lupus erythematosus (SLE) or aPL are urged to avoid combined estrogen- progestin contraception and the transdermal estrogen-progestin patch; the ACR strongly recommends use of an IUD or progestin-only pill.
Women who are at risk for osteoporosis should avoid intramuscular DMPA injections. Assisted reproductive technology
RMD itself generally doesn’t affect fertility, but some drugs (e.g. cyclophosphamide) might. For women with stable, uncomplicated RMD who are aPL negative, the ACR strongly recommends ART. However, women with active RMD should defer ART until the disease is stable/quiescent.
The ACR has made additional recommendations for women with positive aPL who undergo ART:
Embryo and oocyte cryopreservation are strongly recommended for women with unstable RMD, with the following conditional recommendations:
Men with RMD should not use gonadotropin-releasing hormone agonist therapy, and sperm cryopreservation should occur before CYC treatment.
Women with RMD who do not have SLE or aPL can safely use hormone replacement therapy (HRT). The ACR conditionally recommends HRT for women with SLE and negative aPL.
Women with positive aPL have additional recommendations:
GPS dictate that all women receive counseling about pregnancy planning and management, including disease stability, compatible medications, and the importance of collaborations between rheumatology and obstetrics-gynecology/maternal-fetal medicine.
Before pregnancy, the ACR strongly recommends that medications be switched to pregnancy-
compatible alternatives to ensure they’re effective and well tolerated.
Further recommendations for women with SLE:
Anticoagulant therapy should continue for 6-12 weeks post-partum.
In addition, the ACR strongly recommended that women with SLE, SLE-like diseases, Sjögren’s syndrome, systemic sclerosis, or rheumatoid arthritis be tested early for anti-Ro/SSA and anti- La/SSB.
The ACR made several recommendations about use of medications.
1. Men:
2. Women:
The ACR encourages breastfeeding for women with RMD, with the acknowledgement that benefits of disease control need to be balanced with the risk of exposing an infant to medications through breast milk. Hydroxychloroquine, colchicine, sulfasalazine, rituximab, and all TNF inhibitors are compatible with breastfeeding. Drugs that are not compatible with breastfeeding include CYC, leflunomide, MMF, and thalidomide.
Although they may face some unique challenges, women with RMD have a great chance at conceiving and delivering a healthy baby when appropriate precautions are taken. The ACR guidelines repeatedly stressed the importance of having a multidisciplinary health care team that includes specialists from rheumatology, obstetrics-gynecology, and maternal-fetal medicine.
The ACR also emphasized the need for aPL testing among women of reproductive age; a positive aPL test has implications for more than pregnancy. aPL-positive women who use estrogen-based birth control increase their risk for thrombosis. The AVISE APS test is an advanced APS diagnostic test that can help inform reproductive health care strategies for women, whether their goal is contraception or delivering a healthy baby.
References: